By Dr Leena Dhole
BAMS, MS (General Surgery)
Proctosurgeon, Healing Hands Clinic
What is Piles?

How do Piles Affect the Body?
Types of Piles
| Type | Location | Symptoms | Details / Grades |
|---|---|---|---|
| Internal Piles | Forms inside the anal canal; usually not visible. | Usually painless; may cause bleeding during bowel movements |
Grade I: Remain inside; may bleed, no protrusion Grade II: Protrude during bowel movement, return on their own Grade III: Protrude, need manual repositioning Grade IV: Permanently outside, painful and swollen, especially with clots |
| External Piles | Under the skin around the anus. | Painful lumps, especially if irritated or thrombosed; symptoms include pain, itching, swelling | Clearly visible and 00palpable; discomfort increases with clot formation or irritation |
| Prolapsed Piles | Internal piles that have protruded outside the anus | Varying pain and discomfort depending on severity |
Grade II: May retract on their own. Grade III: Require manual repositioning. Grade IV: May remain outside permanently. |
| Thrombosed Piles | Usually, external piles with blood clot formation | Sudden, severe pain, swelling, and sometimes bluish discoloration of the lump | Requires prompt attention; clot can lead to intense inflammation and discomfort |

Causes of Piles?
Understanding the types of piles is just one part of the puzzle. But what actually causes piles in the first place? Let’s break down the common triggers and risk factors:
- Straining while passing stool: This often happens because of constipation and puts extra pressure on the veins in your rectum and anus.
- Ongoing constipation or diarrhea: Chronic digestive issues can irritate the area and lead to swelling over time.
- Sitting for too long, especially on the toilet: This slows down blood flow and puts stress on the rectal veins.
- Being overweight: Extra body weight, especially around the belly, increases pressure on the lower body, including the veins around your anus.
- Pregnancy: The growing uterus puts pressure on abdominal veins, and hormonal changes can slow down digestion, both of which make hemorrhoids more likely.
- Ageing: As you grow older, the tissues supporting the veins in your rectum can become weaker, making them more prone to swelling.
- Lifting heavy weights often: Regularly lifting heavy objects, especially without proper technique, can cause strain that affects the anal veins.
- Low-fiber diet: Not getting enough fiber can lead to hard stools, which make you strain more during bowel movements.
- Genetics and inactivity: If hemorrhoids run in your family, or if you have a mostly sedentary lifestyle, your risk may be higher.
Symptoms of Piles/Hemorrhoids
Recognizing the symptoms early can help you act before things get worse. The symptoms of hemorrhoids vary depending on their type and how severe they are. Common signs of hemorrhoids include:
- Pain or Discomfort: Experiencing pain or discomfort, especially during and after bowel movements, is a common symptom of piles.
- Bright Red Bleeding: You might notice bright red blood either during or after passing stool.
- Itching and Irritation: The anal area can become itchy and irritated.
- Swelling or Lumps: There may be swelling or lumps around the anus, which can be tender or painful when touched.
- Incomplete Evacuation: A feeling that the bowels have not been completely emptied after a movement is another symptom.
In more serious situations, complications may arise, such as significant bleeding (which could lead to anemia), infection, or thrombosis (blood clots occurring in external piles). Some people may experience piles without any noticeable symptoms, while others might find them causing considerable discomfort and impacting their daily life activities.
How is Piles Diagnosed?
If you're noticing any of these signs, you might be wondering, "What now?" Let’s look into how doctors actually diagnose piles or hemorrhoids and determine the right course of action. A proper diagnosis involves several steps to pinpoint the exact nature and extent of the condition:
- Assessment of Medical History: The doctor first gathers information about your symptoms. You'll be asked about your eating and toilet habits, any use of laxatives, and relevant medical history. This helps the doctor understand what is triggering your piles symptoms.
- Physical Examination: If you have external piles, the doctor will examine the area around the anus for lumps, swelling, or irritation. They might also do a digital rectal examination. This involves using a gloved finger to check for internal hemorrhoids, tenderness, or any signs of blood.
- Procedures for Internal Piles: For internal piles, doctors may use special tools, as follows:
- Anoscopy: A short, rigid tube is inserted into the anus to examine the anal canal and lower rectum.
- Sigmoidoscopy: A flexible tube is used to examine the lower part of the colon.
- Colonoscopy: A more comprehensive examination of the entire colon often used when symptoms suggest other gastrointestinal disorders.
Treatment for Piles
When considering treatment for piles or hemorrhoids, there are several options to consider. The right approach depends on how severe your piles symptoms are and how they affect your daily life. Most people start with simple home remedies before moving to stronger treatments.
Early-stage piles often respond well to lifestyle changes and natural remedies. However, if your hemorrhoids symptoms persist or worsen, medical treatments or surgical options might be necessary. Let's explore each treatment category to help you understand what works best for different situations.
Home Remedies and Lifestyle Changes
Home remedies and lifestyle changes form the foundation of piles treatment, especially in the early stages. These natural approaches work by reducing inflammation, easing pain, and preventing the straining that worsens hemorrhoids.
| Remedy | What It Means | How to Follow It |
|---|---|---|
| Warm Sitz Baths | Soaking the anal area in warm water to ease pain and itching | Fill a tub or large bucket with comfortably warm water. Sit in it for 10–15 minutes, 2–3 times a day, especially after a bowel movement. You can also add a pinch of salt for extra relief. |
| Dietary Changes | Eating more fiber to soften stool and avoid constipation | Add fruits like papaya, guava, and bananas; vegetables like lauki, palak, and carrots; and whole grains like atta, daliya, or brown rice. Drink 8–10 glasses of water daily; chaas or nimbu paani also count. |
| Exercise | Daily movement to improve digestion and reduce pressure in the rectal area | A 20–30 minute walk after dinner, climbing stairs at home, or simple yoga like Pavanmuktasana can help in the treatment of piles. Avoid long sitting sessions at work or watching TV. |
| Stool Softeners & Fibre Supplements | Help make stools easier to pass, reducing pain and straining | If home food isn't enough, try Isabgol (psyllium husk) mixed with warm water or milk before bed. You can also ask a doctor about supplements like lactulose or mild fiber powders. |
| Good Toilet Habits | Preventing excess pressure during bowel movements | Don’t scroll on your phone in the toilet. Go when you feel the urge—don’t hold it in. If you're constipated, don’t force it. Squatting posture (or using a small footstool) can also help. |
| Maintain a Healthy Weight | Reducing pressure on rectal veins and preventing new or worsening piles | Avoid high-fat, low-fiber foods. Eat balanced meals and stay active. Losing even a few kilos can help relieve pressure on the pelvic and rectal area. |
| Practice Good Anal Hygiene | Preventing irritation and infection in the anal area | Clean the area gently with warm water after bowel movements. |
Piles Medicines
Medications play a crucial role in managing piles when lifestyle changes and home remedies aren’t enough. Depending on the severity of symptoms and personal preferences, treatment options for piles range from conventional allopathic drugs to gentler, plant-based formulations. Both approaches aim to relieve discomfort, reduce inflammation, and improve bowel function, each with its own advantages and limitations
Over-the-counter (OTC) Medication
Over-the-counter medicines for piles focus on symptom relief through conventional pharmaceuticals. These treatments can be broadly grouped into the following categories:
- Stool softeners and laxatives, such as docusate or lactulose help soften stools and make bowel movements smoother. This reduces the need to strain, easing pressure on swollen veins.
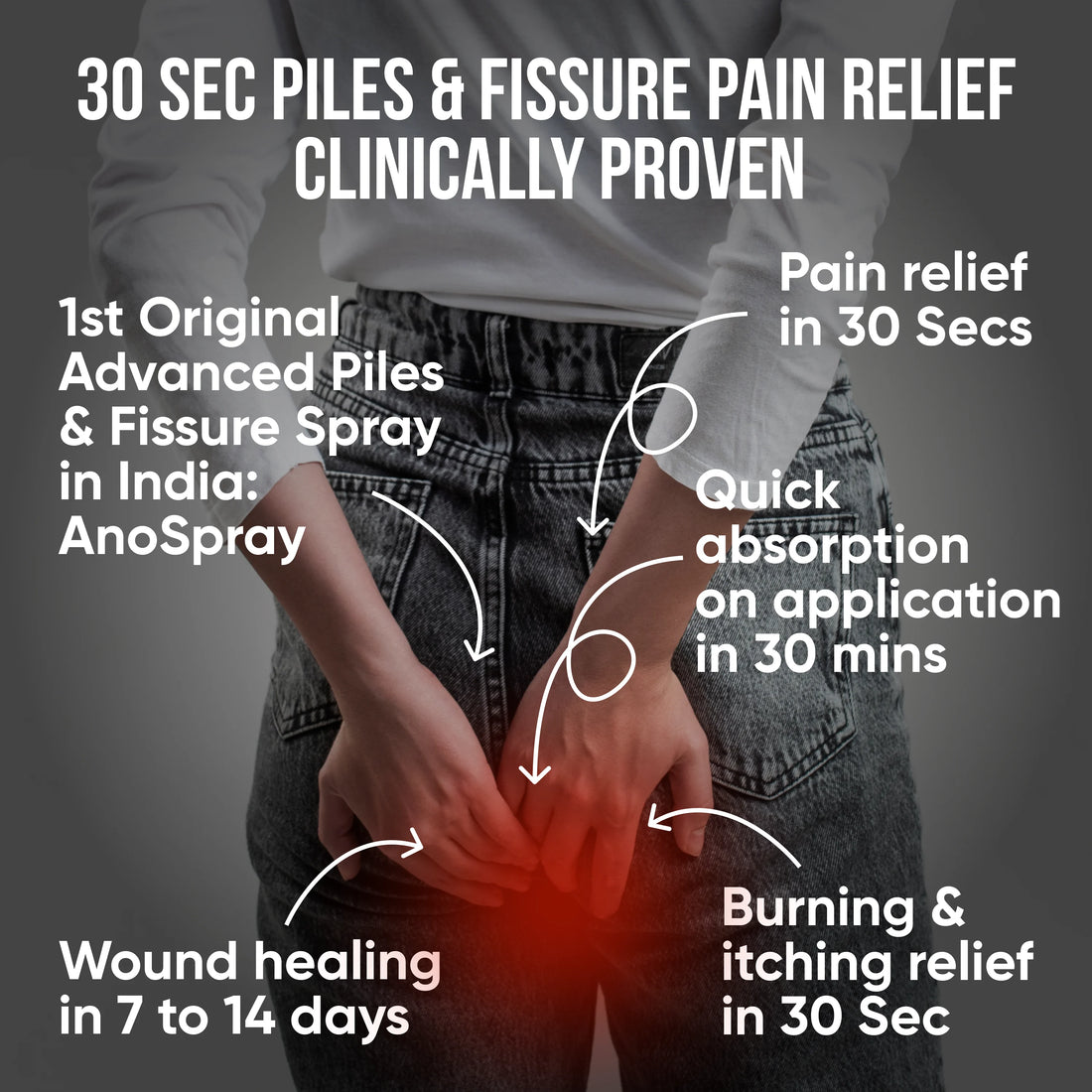
- Topical creams and ointments, containing ingredients like hydrocortisone, lidocaine, or pramoxine help soothe itching, burning, and mild discomfort around the anal area. Unlike regular creams that just numb the pain for a while, Anoac Cream is India’s first patented and clinically proven piles cream that actually helps treat the condition — not just temporarily hide the symptoms.
- Oral pain relievers like ibuprofen or acetaminophen may be used to manage general pain and discomfort temporarily.
These piles medicines offer quick relief but don't address the underlying causes of the symptoms of hemorrhoids, like constipation or poor bowel habits.
Plant-based Medication
With growing awareness, more people are now turning to natural solutions for piles treatment because they want gentler, plant-based approaches. These treatments work with your body's natural healing processes rather than simply masking symptoms. Plant-based formulations offer comprehensive care by addressing multiple aspects of piles. For instance, PiloKit by Healing Hands is a three-part patented plant-based formulation that addresses piles from multiple angles, relieving symptoms, promoting healing, and tackling the root cause:
- PiloSpray: PiloSpray is a topical spray designed for hygienic, no-contact application, which is ideal for those experiencing pain, bleeding, or itching during flare-ups. Its plant-based ingredients help reduce inflammation and discomfort while also supporting wound healing and infection control. The ease of use and soothing action make it especially helpful for people who struggle with the discomfort of direct application.
- PiloTab: PiloTab works from within, targeting both internal and external piles. It helps shrink the piles mass, reduces inflammation, and minimizes bleeding. More importantly, it aids in tissue repair, supporting long-term healing rather than offering just temporary relief. This internal approach complements topical solutions, addressing the condition from the inside out.
- ConsteTab: Constipation and straining are major triggers for piles. ConsteTab helps address this root issue by acting as a natural stool softener and mild laxative. Made with plant-based ingredients, it supports smooth bowel movements without the harsh effects of chemical laxatives. Regular use can help maintain digestive balance and reduce pressure on anal veins.

Why Consider Plant-based Medicine for Piles?
Plant-based treatments offer a gentle, effective alternative to harsh or invasive options. Healing Hands’ clinically validated Ayurvedic medicine for piles is formulated using ayurvedic principles that focus on the root causes, such as poor digestion and imbalances in daily habits but validated with clinical research. These medicines are entirely plant-based and developed into India’s first patented and clinically validated kits. This holistic approach not only reduces discomfort and inflammation but also supports long-term digestive health, offering relief the natural way.
Surgery Options
If home remedies and medications aren't effective, surgical options, like stapled hemorrhoidopexy, laser hemorrhoidoplasty, and others might be considered for the treatment of hemorrhoids. Here are some options:
Stapled hemorrhoidopexy
Stapled hemorrhoidopexy is a modern surgical technique for treating internal hemorrhoids. The procedure involves cutting off blood supply to the swollen tissue using surgical staples. This causes the piles to shrink and eventually disappear.
During the procedure, the surgeon repositions the hemorrhoidal tissue back to its normal location and staples it in place. This reduces the prolapse (bulging) that causes discomfort and bleeding.
Laser Hemorrhoidoplasty (LHP)
Laser hemorrhoidoplasty (LHP) involves the use of focused laser energy to coagulate hemorrhoids, causing them to shrink gradually. The laser seals blood vessels feeding the swollen tissue, cutting off its blood supply without removing the tissue entirely.
This minimally invasive procedure causes less trauma to surrounding tissues than does conventional surgery. The precision of laser technology allows surgeons to target only the affected areas while preserving healthy tissue. Most patients experience minimal bleeding and faster recovery times.
Laser treatment for piles is particularly suitable for people who want to avoid the discomfort associated with traditional surgical removal.
Other treatment procedures
The below procedures are less common but available alternative treatment options for piles:
- Rubber Band Ligation: A tight rubber band is placed around the base of the hemorrhoid to cut off blood supply. The hemorrhoid dries up and falls off in a few days. It’s quick and usually done without anesthesia.
- Sclerotherapy: A chemical solution is injected into the hemorrhoid, making it shrink over time. It’s mostly painless and used for smaller internal piles treatment.
- Infrared Photocoagulation or Electrocoagulation: These methods use heat or electric current to destroy hemorrhoidal tissue and reduce its size. They’re done in clinics and are suitable for internal piles that don’t respond to basic treatment.
Note: minimally invasive procedures like sclerotherapy and infrared coagulation are sometimes used, although they're not considered standard care nowadays. These techniques may offer temporary relief but often require repeat treatments and don't address the underlying problem as effectively as newer surgical methods.
When to See a Doctor
Even with the best prevention strategies, there are times when medical attention is necessary. So how do you know when it’s time to seek help?
- Your piles symptoms don’t get better with home treatment or start getting worse.
- You have significant pain, swelling, or bleeding.
- There's a lump near your anus that doesn’t get better or causes serious discomfort.
- You notice changes in how often you go to the bathroom, stool color, or consistency. If rectal bleeding comes with dizziness or fainting, it could indicate something more serious like colorectal cancer.
- There are signs of complications, such as severe pain, infection, or prolapsed tissue that can't be pushed back in.
Many people in India postpone medical care for anorectal conditions due to stigma or fear of procedures. However, piles treatment has evolved significantly, and most cases can be managed effectively with minimally invasive approaches.
Questions to Ask Your Doctor
When you visit your doctor for piles, asking the right questions helps you understand your condition and treatment options better. Here is a list of questions that will help you understand your condition better:
- What type of hemorrhoids do I have — internal or external?
- What lifestyle changes should I make to prevent recurrence of piles?
- Are there specific foods I should avoid or include in my diet for piles management?
- What over-the-counter piles medicine is safe for me to use?
- When should I consider medical or surgical procedures for piles treatment?
- What signs indicate my condition is getting worse?
Complications from Untreated Piles
While piles are generally not dangerous, untreated cases can lead to complications that may affect your quality of life. Below are some complications that can result from a delay in hemorrhoid treatment:
- Anaemia from Ongoing Bleeding: Frequent bleeding may lead to low iron levels over time, causing tiredness or weakness, especially if your diet is already lacking in iron.
- Strangulated Hemorrhoid: In rare cases, a prolapsed hemorrhoid may lose its blood supply, leading to increased pain.
- Risk of Infection: Poor hygiene or open wounds from severe piles can increase the chances of infection.
- Persistent Prolapse: Sometimes, hemorrhoids may remain outside the anus, causing daily discomfort.
Find Long-Lasting Relief from Piles
While quick fixes may offer temporary comfort, true healing from piles comes from addressing the underlying causes. By following a fiber-rich diet, staying active, adopting good toilet habits, and maintaining anal hygiene, you can take meaningful steps toward long-term relief.
And if you need gentle, plant-based support along the way, PiloKit is here for you. This patented 3-step formulation works holistically to relieve symptoms, promote healing, and support your body’s natural recovery process—without harsh chemicals or invasive procedures.
Don’t just manage the discomfort, choose a solution that supports lasting well-being from the inside out.
FAQs
1. What are piles and how do they differ from other anorectal conditions?
Piles, also known as hemorrhoids, are swollen blood vessels in the rectal area. Unlike fissures or fistulas, piles involve enlarged veins that can occur inside the rectum or around the anus, causing discomfort and bleeding.
2. What are the main causes of piles that I should be aware of?
The primary causes of piles include chronic constipation, straining during bowel movements, prolonged sitting, low-fiber diet, pregnancy, and obesity. These factors increase pressure on rectal veins, leading to swelling and inflammation of the blood vessels.
3. How can I recognise piles symptoms early to seek timely treatment?
Common piles symptoms include bright red bleeding after passing stools, itching around the anus, pain or discomfort, feeling of incomplete bowel evacuation, and visible lumps near the anal opening during flare-ups.
4. What treatment for piles options are available for managing this condition?
Piles treatment includes dietary changes with increased fiber intake, adequate hydration, warm sitz baths, topical ointments, and lifestyle modifications. Severe cases may require medical procedures, but early-stage piles often respond well to conservative management approaches.
5. Are there effective piles medicine options that can provide relief at home?
Yes, medicines for piles include topical creams with anti-inflammatory properties, pain-relief ointments, stool softeners, and plant-based formulations such as PiloKit. However, consulting a doctor before starting any piles medicine ensures safe and appropriate treatment for your specific condition.
6. What lifestyle changes can help prevent piles from coming back?
Preventing piles recurrence involves adopting daily habits that support healthy digestion and reduce pressure on rectal veins. This includes eating a high-fiber diet, drinking plenty of water, avoiding prolonged sitting or straining on the toilet, staying physically active, maintaining a healthy weight, and practicing good anal hygiene. These habits not only prevent piles but also improve overall gut health.
7. Are symptoms of piles in males different from symptoms of piles in females?
Hemorrhoid symptoms are generally the same for all genders and are often linked to poor lifestyle and dietary habits. Common signs include pain or discomfort during bowel movements, itching or irritation around the anus, swelling near the anal area, bleeding while passing stool, and the presence of a painful or tender lump near the anus. Addressing the underlying causes—like constipation, prolonged sitting, or low-fiber diets—can help manage and prevent these symptoms effectively.
8. Can exercise help with managing piles symptoms?
Yes, regular exercise like walking or swimming can help improve digestion and reduce symptoms of piles by preventing constipation and reducing pressure on veins.
9. How can I prevent hemorrhoids (piles) during pregnancy?
To help prevent hemorrhoids during pregnancy, make sure to drink plenty of water and eat a diet rich in fiber (like fruits, vegetables, and whole grains). Staying active with light exercises such as walking can improve digestion and ease pressure. Avoid straining while passing stools by not delaying bathroom visits and using good toilet posture. Following these habits can significantly reduce your chances of developing hemorrhoids during pregnancy.
10. Are there any risks associated with untreated piles?
If left untreated, piles can lead to complications like chronic blood loss leading to anemia, severe pain, or infection around the anus, which might require medical intervention.
11. How long do piles take to heal?
Early stage piles may clear up in a few days with lifestyle changes and timely treatment with proven piles medicines like PiloKit, while larger external piles may take longer. Persistent symptoms should be evaluated by a doctor.
12. Is Healing Hands’ Ayurvedic medicine for piles clinically tested?
Yes. Healing Hands offers India’s first patented and clinically validated plant-based kit PiloKit for piles, combining the safety of natural ingredients with the credibility of modern research.
References
https://www.mayoclinic.org/diseases-conditions/hemorrhoids/symptoms-causes/syc-20360268
https://my.clevelandclinic.org/health/diseases/15120-hemorrhoids
https://pubmed.ncbi.nlm.nih.gov/24881480/
https://emedicine.medscape.com/article/775407-overview
https://www.webmd.com/digestive-disorders/understanding-hemorrhoids-basics
https://www.healinghandsclinic.co.in/piles-mulvyadh-bavasir-treatment/
https://myhealinghands.in/products/pilokit-complete-piles-treatment-kit-30-days
 Piles, Fissure & Fistula Medicine
Piles, Fissure & Fistula Medicine
 Constipation Care
Constipation Care
 Acidity Care
Acidity Care
 IBS & Gut Health
IBS & Gut Health
 Healing with Turmeric
Healing with Turmeric