By Dr. Namita Ambike
BAMS, Consulting Physician
Healing Hands Clinic

What is Anal Fissure?
An anal fissure is a small tear in the delicate lining of your anus. This tiny cut also known as fissure in ano, causes sharp pain, burning and bleeding when you pass stool. It is a common condition that can happen to people of all ages. It is often triggered by constipation and straining during bowel movements.

How do Anal Fissures Affect the Body?
Your anus sits at the end of your digestive tract, where stool leaves your body. A strong ring of muscle called the anal sphincter surrounds this opening, helping you control bowel movements.
When a fissure in the anus develops, it creates an open wound that exposes the underlying muscle. This exposure causes painful muscle spasms every time you have a bowel movement. The pain can be sharp and burning, often lasting several hours after you finish.
These spasms create a bigger problem. They reduce blood flow to the torn area, making it harder for your body to heal naturally. This is why some fissures become chronic and refuse to heal on their own.
Anal fissure symptoms become worse because passing stool reopens the tear repeatedly. The whole process disrupts your normal routine. The pain makes you dread using the toilet, which often leads to holding in the stool. This creates harder stools, more straining, and a cycle that makes the fissure worse.
Types of Fissures

Anal fissures are classified into two types based on how long they've been present and what changes have occurred in the tissue.
Acute Anal Fissure
An acute anal fissure is a recent tear that causes sharp, burning pain during and after bowel movements—often described as passing broken glass. The pain can last from minutes to hours. Most acute fissures heal on their own within weeks.
Chronic Anal Fissure
A chronic anal fissure lasts over six weeks, with thickened edges, a sentinel pile, and sometimes visible muscle at the base. Pain is more persistent, with frequent spasms. It usually won’t heal with home care alone and needs medical attention.
Here is a table to show the difference between the two types of anal fissure:
| Feature | Acute Anal Fissure | Chronic Anal Fissure |
|---|---|---|
| Duration | Recent tear, present for less than 6 weeks | Persists for more than 6–8 weeks |
| Cause | Usually due to passing hard or large stools, diarrhea | Poor healing from repeated or prolonged strain, diarrhea |
| Pain | Sudden, sharp, burning pain during or after bowel movement | Persistent, less sharp pain; may interfere with daily activities |
| Appearance | Fresh tear with smooth edges | Thickened, scarred edges; possible sentinel skin tag |
| Muscle Spasm | Present but usually temporary | Ongoing internal sphincter spasm restricts blood flow |
| Healing Response | Heals naturally in most cases with simple care | Difficult to heal without medical intervention |
| Treatment | Diet changes, hydration, sitz baths, medication | Fissure medicine, minor surgical procedures (if needed) |
| Prognosis | Excellent with early management | Requires targeted therapy to break the cycle of non-healing |
Causes of Fissures
- Hard or large stools: When you're constipated, passing hard stools forces your anal lining to stretch beyond its limits. This stretching tears the thin tissue, creating a fissure. The anal mucosa is much more delicate than regular skin, making it prone to injury.
- Straining during bowel movements: Excessive pushing increases pressure in your anal canal. This pressure can cause existing small tears to worsen or create new ones in the anal lining.
- Chronic diarrhea: Frequent loose stools irritate and inflame your anal canal. This constant irritation weakens the tissue, making it more likely to tear even with normal bowel movements.
- Childbirth trauma: Vaginal delivery can stretch and damage the anal area, especially during prolonged labour or when delivering larger babies. This makes new mothers more vulnerable to developing fissures.
- Inflammatory bowel diseases: Conditions like Crohn's disease cause ongoing inflammation in your intestines. This chronic inflammation weakens your anal lining and increases your risk of developing fissures.
- Physical trauma: Anal intercourse, medical procedures, or insertion of foreign objects can directly injure the anal lining and create tears.
- Poor hygiene or infections: Infections or irritation from harsh cleaning products can inflame your anal skin, making it more susceptible to tearing.
- Age-related factors: Infants and adults between the ages of 40 and 60 are more prone to anal fissures because their anal tissue tends to be more delicate or less elastic. In infants, the tissue is still developing, while in middle-aged adults, reduced blood flow and natural aging can make the skin more susceptible to tearing.

What are the Risk Factors for Anal Fissure?
- Constipation and straining: This is the primary risk factor. When you strain to pass hard stools, you create excessive pressure that can tear your anal lining.
- Age vulnerability: Infants have naturally delicate anal tissue, whilst middle-aged adults experience changes in tissue elasticity that make fissures more likely.
- Recent childbirth: Women who've had vaginal deliveries face a higher risk due to stretching and potential trauma to the anal area during birth.
- Inflammatory bowel diseases: Crohn's disease and similar conditions create chronic inflammation that weakens your anal tissues over time.
- History of anal trauma: Previous injuries or medical procedures in the anal area can create scar tissue that's more prone to tearing.
- Poor bowel habits: Delaying bowel movements when you feel the urge allows stools to become harder and more difficult to pass.
- Low-fibre diet: Diets lacking adequate fruits, vegetables, and whole grains lead to harder stools that require more straining to pass
Symptoms of Anal Fissures
- Severe pain during bowel movements: You'll experience sharp, intense pain that many describe as feeling like passing glass or knives. This pain occurs during defecation and can last for minutes to hours afterwards.
- Bright red bleeding: You'll notice fresh blood on toilet paper, in the toilet bowl, or on the surface of your stool. Unlike other conditions, fissure bleeding is typically bright red and occurs with bowel movements.
- Anal itching and irritation: The area around your anus may feel itchy, burning or irritated due to inflammation and the body's healing attempts.
- Visible tear or skin tag: You might see a small crack in the anal opening or notice a small piece of skin (sentinel pile) near the fissure site.
- Anal muscle spasms: Your anal sphincter muscle may go into spasm, causing additional cramping and discomfort that can persist between bowel movements.
The pain from fissures tends to be sharp and episodic, occurring mainly with bowel movements. This differs from hemorrhoid pain, which can be more constant and throbbing.
In infants, symptoms of fissure may appear as unusual fussiness during nappy changes and blood streaks in their stool.
These symptoms often worsen with poor dietary habits or dehydration, making early recognition and treatment for fissures essential.
How is Fissure Diagnosed?
Proper diagnosis of a fissure requires a thorough medical evaluation to distinguish it from other anal conditions and determine the best treatment approach. Let's take a look at the pointers below:
Symptom Review
Physical Examination
Endoscopy Procedures
Your doctor may also do some endoscopic exams to ensure accurate identification and appropriate fissure treatment planning
Anoscopy
Sigmoidoscopy
This examines your lower colon and rectum if deeper inflammation is suspected, particularly useful when inflammatory bowel disease might be present.Colonoscopy
A comprehensive examination of your entire colon is recommended when bleeding persists or other intestinal diseases need to be ruled out.
Treatment for Anal Fissures
Fissure treatment focuses on breaking the painful cycle that prevents healing. When you have an anal fissure, the torn tissue struggles to repair itself because muscle spasms and pain during bowel movements keep reopening the wound. Treatment options range from simple home care to medical interventions, all aimed at reducing pain, softening stools, and allowing natural healing to occur.
Home Remedies
Simple home remedies can provide significant relief for fissure symptoms and promote natural healing. These approaches focus on reducing strain during bowel movements, keeping stools soft, and creating conditions that support tissue repair. Many of these remedies align well with traditional Indian practices and can be easily incorporated into daily routines. Key home remedies include:
| Remedy | Details |
|---|---|
| Increase dietary fibre intake | Add more whole grains, fruits like papaya and guava, vegetables such as spinach and carrots, and legumes to your meals. Aim for 25–30 grams of fibre daily to soften stools naturally. Fibre absorbs water and creates bulk, making bowel movements easier and reducing trauma to the fissure in anus. |
| Stay well hydrated | Drink 2–3 litres of water daily, including herbal teas and buttermilk. Proper hydration keeps stools soft and prevents the straining that worsens anal fissure symptoms. Water works with fibre to create the right stool consistency for comfortable passage. |
| Take warm sitz baths | Soak the affected area in warm water for 10–15 minutes, especially after bowel movements. This relaxes the anal muscles, improves blood flow to promote healing, and provides immediate pain relief. The warmth reduces muscle spasms that often accompany fissures. |
| Avoid straining during bowel movements | Respond to the urge promptly and don't spend long periods on the toilet. Use a footstool to elevate your feet, which improves the angle for easier stool passage. Straining increases pressure on the fissure and delays healing. |
| Maintain gentle anal hygiene | Clean the area with plain water after bowel movements and pat dry gently. Avoid harsh soaps or fragranced wipes that can irritate the sensitive tissue. Water-based cleaning helps prevent infection whilst being gentle on healing skin. |
| Use natural stool softeners | Psyllium husk (isabgol) mixed with water creates bulk and softness, reducing the mechanical trauma during defecation. Take it regularly to maintain a consistent stool texture. |
| Moderate spicy foods | Whilst healing, reduce very hot spices that may increase discomfort during bowel movements. This gives the fissure time to heal without additional irritation. |
Medications
Over-the-counter Medication
OTC fissure medicine aims to break the pain-spasm cycle. These treatments can be broadly categorised into the following categories:
- Topical anaesthetics like lidocaine numb the area during bowel movements, providing immediate pain relief. Some creams contain vasodilators like nitroglycerin, which relax the internal anal sphincter muscle and increase blood flow to promote healing. However, these are temporary solutions which do not provide proper treatment and are not ideal for long term use, as they can cause headache, dizziness in some users due to their effects on blood vessels.
- Stool softeners such as docusate sodium prevent the hard stools that can reopen healing fissures. Bulk-forming fibre supplements like psyllium husk help maintain soft stools consistently, preventing further trauma to the healing fissur

Plant-based Medication
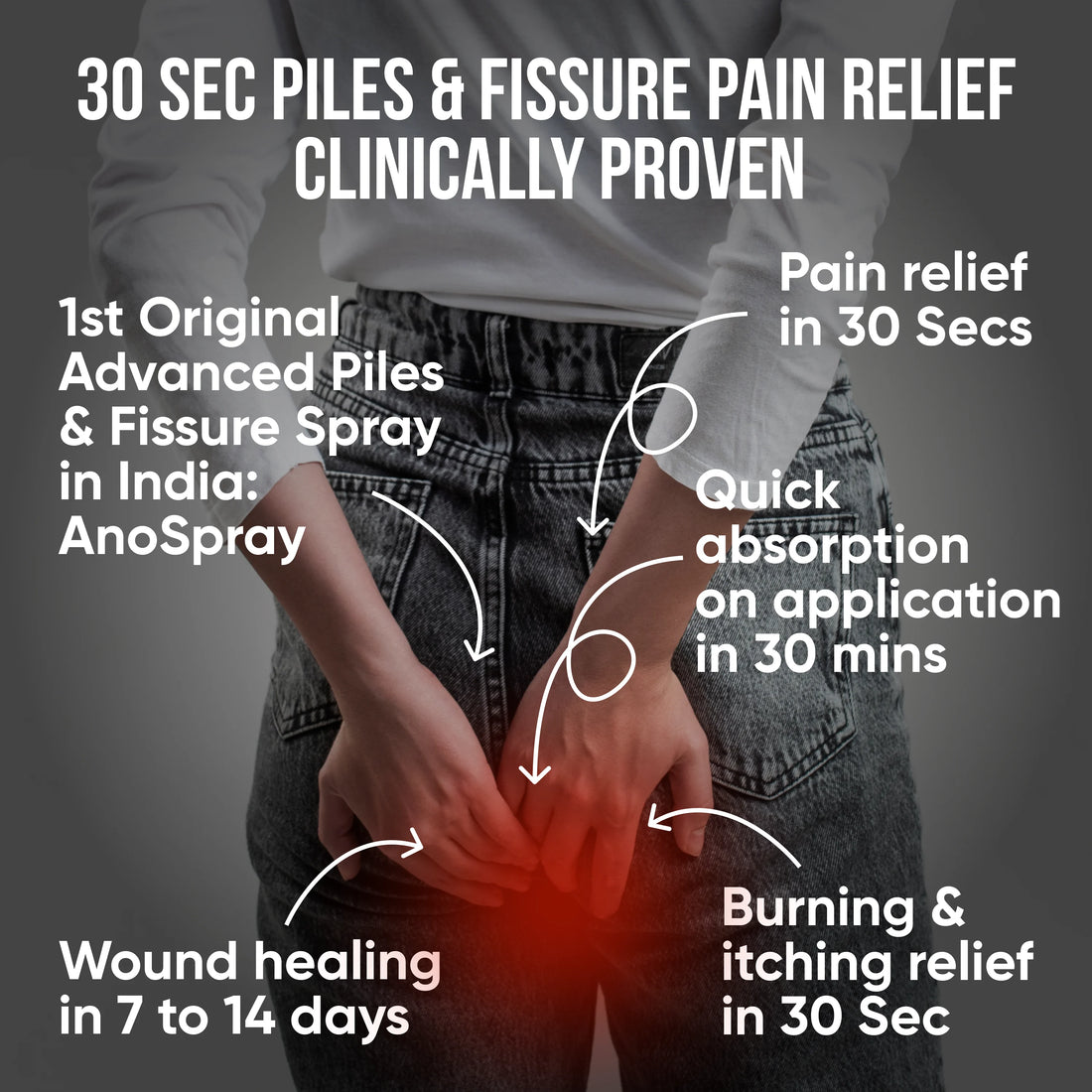
- PiloSpray: This herbal topical spray delivers fast relief from pain and burning sensations through natural anti-inflammatory agents. The spray format maintains hygiene whilst providing targeted application to the sensitive anal area. Its plant-based formula promotes tissue healing without harsh chemicals, making it suitable for regular use during the healing process.
- PiloTab: These oral tablets contain plant extracts specifically chosen to improve blood circulation and reduce inflammation around the fissure site. Better circulation brings nutrients and healing factors to the damaged tissue, whilst reduced inflammation lessens pain and swelling. The tablets also help strengthen the anal mucosa, making it more resistant to future tears.
- ConsteTab: Designed to address constipation—a primary cause of anal fissure—these tablets contain natural laxatives and fibre-rich herbs. They work gently to soften stools and promote regular bowel movements without creating dependency. By preventing the hard stools that cause fissures, ConsteTab helps break the cycle of injury and re-injury.
Surgery Options
When an anal fissure becomes chronic—lasting more than 6-8 weeks—and doesn't respond to conservative treatment, surgical intervention may be necessary. Surgery aims to reduce muscle spasm, improve blood flow to the fissure site, and create conditions for proper healing. The choice of procedure depends on fissure severity, patient health, and surgeon expertise. At Healing Hands Clinic we have specialised well trained surgeons to treat patients with such conditions.
Partial Lateral Internal Sphincterotomy (PLIS)
Laser Surgery
Botulinum (Botox) Injection
Lord's Dilatation
When to See a Doctor
- Bright red blood on toilet paper or in stools that persist beyond 6 – 8 weeks
- A visible crack or tear around your anal opening
- Symptoms of fissure continuing for more than 6 – 8 weeks despite trying home remedies
- Fever, pus discharge, or swelling around the anal area
- Pain so intense that you avoid bowel movements entirely
Complications from Untreated Anal Fissures
- Anal sphincter spasm: The muscle around your anus tightens to protect the area, reducing blood flow and preventing natural healing.
- Infection: Bacteria can enter the tear, potentially causing abscesses or fistulas that may require surgical intervention.
- Skin tags: Chronic fissures often develop small skin flaps near the tear, creating hygiene challenges and discomfort
In India, delayed treatment due to embarrassment often worsens these fissure complications. The anal sphincter spasm creates a cycle where pain leads to muscle tension, which further reduces healing. This is why early intervention with proper medicines for fissure or lifestyle changes is crucial.
Without treatment, you might eventually need anal fissure surgery, which could have been avoided with timely care with proven medicines and appropriate home management.
Your Path to Healing: Managing Fissures Effectively
FAQs
- What is a fissure in the anus and what are the types of anal fissure?An anal fissure is a small tear in the anal canal lining causing pain during bowel movements. There are two types: acute fissures (heal within 6-8 weeks) and chronic fissures (persist longer, requiring medical and surgical treatment).
-
What causes anal fissure and why do they develop?
The main causes of anal fissure include passing hard, dry stools due to constipation, prolonged diarrhoea, childbirth strain, excessive straining during defecation, and inflammatory bowel conditions. Poor fiber intake commonly contributes to fissure development. -
What are the main symptoms of fissure and how to identify anal fissure symptoms?
Key symptoms of fissure include severe, sharp pain during and after bowel movements, bright red bleeding on stool or tissue, burning and itching around the anus, and visible tears. Pain often lasts minutes to hours after defecation. -
What are effective home remedies for fissure and how to cure fissure at home
Effective home remedies include increasing fiber intake through vegetables and fruits, drinking plenty of water, taking warm sitz baths 2-3 times daily, avoiding straining, and maintaining regular bowel habits to promote natural healing. -
What fissure medicine and treatment options are available, including Ayurvedic medicine for fissure?
Treatment for fissure includes topical ointments like nitroglycerin, stool softeners, and pain relievers. Healing Hands FissureKit Ayurvedic medicines combination for fissure focuses on clinically proven patented plant-based formulations. Severe cases may require anal fissure surgery to prevent fissure complications. Fissure medicines like FissureKit can also be taken for post-surgery recovery for faster healing. -
Are anal fissures permanent?
No. Most acute fissures heal completely with timely treatment with poven medicines like FissureKit. Chronic fissures need medical and surgical treatment. -
Can stress cause anal fissures?
Indirectly, yes. Stress can affect digestion and bowel habits, which may contribute to constipation or diarrhea—both risk factors for fissures. -
How do I know if I have a fissure or hemorrhoids?
Fissures cause sharp pain during bowel movements burning sensation and bleeding; hemorrhoids typically cause swelling, itching, and painless bleeding. -
Is surgery necessary for every fissure?
No. Surgery is only needed for chronic fissures that don’t heal with medication or home care. -
Can I use over-the-counter creams for fissures?
Yes, Anoac cream can reduce pain and inflammation, but for complete treatment we recommend FissureKit which helps with both external and internal anal fissure treatment. -
Is an anal fissure a sign of cancer?
No. Fissures are not cancerous. But persistent symptoms should be evaluated to rule out other conditions. -
Can children get anal fissures?
Yes, especially if they suffer from constipation. Most heal with stool softeners and dietary changes. -
Can I exercise with an anal fissure?
Gentle exercises like walking or yoga are fine. Avoid intense workouts until healing occurs.
-
Can anal fissures come back after healing?
Yes, especially if constipation returns or bowel habits are not managed properly.
 Piles, Fissure & Fistula Medicine
Piles, Fissure & Fistula Medicine
 Constipation Care
Constipation Care
 Acidity Care
Acidity Care
 IBS & Gut Health
IBS & Gut Health
 Healing with Turmeric
Healing with Turmeric